It’s maternal mental health awareness week so here I am, ready to spread some awareness.

For those of you who have had a baby, or who have undertaken the journey of trying to have a baby, you know how full of emotional and mental pitfalls that path can be.
For those of you who haven’t, you may have had a front-row seat to a loved one’s journey. You’re curious about how to talk to a new mom about therapy. Or maybe you’re just one of those dedicated learners who like to gain knowledge and be armed with information for your future. Cheers to you!
The postpartum period seems to finally be getting its time in the spotlight, as so many more people are willing to talk about postpartum depression. As a mental health professional, it’s a relief to see mothers seeking the postpartum support they need.
Furthermore, It’s Important for Those Seeking Postpartum Support in St. Louis, MO to Know…
(Maternal mental health at all stages is important—critical, even. Our St. Louis postpartum therapists partner with women at any stage in motherhood to address concerns around anxiety, depression, overwhelm, relationship tension, parenting teenagers, and so much more. We have specialized training aimed to provide you with the best techniques to address symptoms and get you feeling better. Read our website to see how we do that and check out this blog on maternal overwhelm if that sounds like something that might exactly explain what you’re feeling…..otherwise, for the rest of this blog, we will be specifically addressing the postpartum period.)
But also as a mental health professional, I want to open the gates of knowledge all the way and urge people to know a few crucial things about mental health & postpartum support in St. Louis.

#1: It’s more than just depression that can come up during this period.
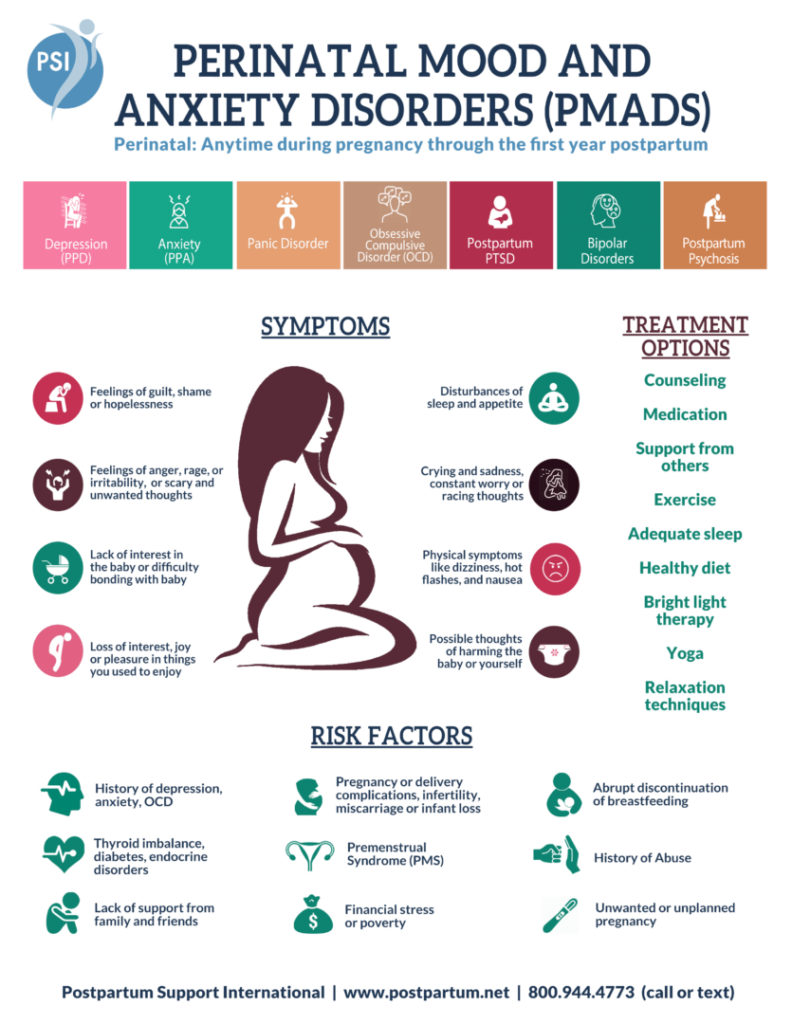
While people commonly use the term “postpartum depression” or “PPD” for mental health symptoms after birth, there’s a host of mental disorders that can arise: anxiety, OCD, bipolar, psychosis, and PTSD. The larger umbrella term is “PMADs” or “perinatal mood and anxiety disorders.”
(To see the full list of PMADs, as well as their symptoms, see the bottom of this post.)
It’s more than just feeling “off” and you know it
It’s so important to recognize this because if you feel “off” but your symptoms don’t match what you know about depression or what you’ve looked up about PPD, that doesn’t mean that what you’re going through is normal or something you have to continue to struggle with in silence. It could be that what you’re going through is a different perinatal mood disorder. Instead of thinking, “Well, I know this isn’t depression so this must just be motherhood” you can realize that something else is at play, that you can get postpartum support, and that alleviation of symptoms is definitely on the table for you!
#2: It’s not just the immediate postpartum period we should be seeking postpartum support for.
Symptoms of PMADs can occur in the days after birth through 12 months postpartum! Which means they can last beyond the baby’s first birthday.
They can also crop up during the pregnancy period before a mom is even at the labor & delivery stage. It’s that symptoms can crop up during pregnancy that the term “perinatal” is what the “P” stands for in “PMADs.” It’s also just more accurate. This means, similar to the point in #1, that you don’t have to tell yourself this is “just how pregnancy is” if you’re feeling off. Anxiety, depression, OCD, or bipolar symptoms may be surfacing and that’s why you are feeling out of control, “not right”, “just not like yourself”, or just out of sorts. Treatment for these symptoms is absolutely an option while pregnant.
Here is what you can do to get postpartum support in St. Louis, MO
To get that postpartum support, open up a conversation with your OBGYN, midwife, or doula. Cruise is a local moms’ group on Facebook. Reach out to a postpartum depression therapist. Try googling “perinatal psychiatrist near me.” Check out Postpartum Support International’s website. There are more resources out there than you may realize (and I can especially attest to wonderful mom resources in St. Louis!) and more popping up every day. Start the conversation and I can almost guarantee you will find results.
#3: It’s not just women who are at risk of these mood disorders; dads are at risk, too!
Research indicates that 1 in 10 dads experience a mood and anxiety disorder. And that’s just of those who report, so the numbers are probably actually a little bit higher.

So, if you’re an STL dad or father in Chicago or St. Louis, MO who is experiencing some challenges around a new baby–whether it’s your first or otherwise–know you are not alone AND that this is absolutely something a postpartum depression therapist can help with. Your life is greatly impacted, too, by the birth of a baby! If you’re the primary financial provider, that’s weighing on you. If you’re the at-home caregiver, your work has just increased. You might wonder how you can keep tending to your marriage AND love another kid. How are you going to coach soccer for your 6-year-old and be present for changing diapers? Are you enough? Can you continue to be enough?
The answer, of course, is yes! But it’s okay if you’re hearing those questions bounce around in your head and it’s okay if you want someone to help you figure out how to answer them.
What puts you at risk for postpartum depression (or other PMADs?)
Certain factors can increase the likelihood of experiencing perinatal mood and anxiety disorders (PMADs). For example, if you’ve had a history of anxiety, depression, or other mental health challenges, you may be more vulnerable. A traumatic birth experience, pregnancy complications, or challenges during labor and delivery can also play a role. Hormonal changes, lack of support from a partner or family, financial stress, or a previous struggle with postpartum symptoms may add to the risk. It’s important to note that PMADs don’t discriminate—any parent can experience them, even if none of these factors apply. Awareness of these risks can help you or your loved ones seek help sooner, creating a smoother path to healing.
So what to do if any of these symptoms are present for you (if you are pregnant or postpartum) or if you observe them in someone else who is pregnant or postpartum)?
If you observe them in another person, gently start a conversation with that person about what you’ve noticed. Let them know you’ve done some research and they shouldn’t have to put up with this alone. Encourage them to talk to a professional can start with their primary care doctor or OBGYN-or can call a postpartum depression therapist. Chiropractors, doulas, sleep specialists, lactation specialists, and a host of other professionals can also point moms in the direction of appropriate help.
If you notice these symptoms in yourself, start the same conversation with the above professionals. If it seems too hard to have the conversation (you’re nervous about crying; it’s tough to describe the symptoms out loud; a phone call or face-to-face conversation is too overwhelming as a starting place), use email or your doctor’s health portal to type out a message. Sometimes, that can feel less intimidating but still allows you to let someone know what is going on.

And here’s what else I absolutely want you to know about Postpartum Support and PMADS:
PMADs are absolutely treatable and they are not your fault! Through medication, in-person or online therapy, or a combination of both, symptom alleviation is truly within reach.
Therapy approaches for perinatal mood and anxiety disorders are often about behavioral, cognitive, and mindfulness habits that can be helpful across the lifespan. And “helpful across the lifespan” is (at least in my opinion) one of the greatest things about therapy! What you learn in that time and how you can shift your relationship with yourself is not going to be time-limited to the perinatal period of your life. You’ll be able to apply those skills, not least amongst them self-compassion, in times of high tide and low tide across the years.
These postpartum support options go for those dads, too: therapy, medication, and maybe a combination of both. For them, also, it’s treatable and not their fault.
Each new baby brings changes to your sense of self, your household operations, and how you interact with those around you. And with changes to those elements of your day-to-day life, comes the possibility, and very real likelihood, that your emotional health will be impacted. Take this new awareness with you on your journey, or with you as you watch others on their journey. Be there for yourself, be there for others, and use this education to makeover motherhood.
Talk to you soon!
Signs and Symptoms of PMADs
Baby Blues
- Tearful
- Reactive
- Primary Emotion: happiness
- Typically resolves after about 2 weeks
Postpartum Adjustment/Postpartum Stress Syndrome
- Lasts longer than 3 weeks
- Can cause feelings of postpartum anxiety/self-doubt
- Deep sadness, without periods of happiness
- Function well & get through the day, but feel awful inside
Perinatal & Postpartum Depression
- Sadness, Crying
- Irritability & Anger
- Hopelessness & Helplessness
- Guilt & Shame
- Suicidal Thoughts
- Appetite Changes & Sleep Disturbances
Postpartum Anxiety
- Agitated & Irritable
- High Alert
- Constant Worry & Racing Thoughts
- Inability to Sit Still
- Shortness of Breath & Heart Palpitations
- Appetite Changes & Sleep Disturbances
Perinatal OCD
- Intrusive, repetitive thoughts (often of harm coming to the baby)
- Overwhelming guilt & shame
- Horrified by your own thoughts
- Hypervigilance
- Engage in behaviors to avoid harm or minimize triggers
Perinatal PTSD
- Flashbacks of events (usually labor & delivery, in this case)
- Recurrent dreams/nightmares
- Avoidance of triggers
- Distressing memories, thoughts, feelings, or external reminders of an event
- Isolation from family/friends/providers
- Distorted sense of blame of self or others
- Numbing
- Hyperarousal/hypervigilance
Perinatal Bipolar I
- Elevated mood symptoms
- Euphoria or agitation
- Decreased need for sleep
- Racing thoughts
- Increased productivity noticed by others
- Pressured speech
- Increased energy
- *Hypomania lasts 4 days
- *Mania lasts 7+ days
Perinatal Bipolar II
- Often mistaken as postpartum depression
- Mood swings/hypomania but only lasts for 1-2 days
- Irritability, hostility
- Racing thoughts
- Psychomotor retardation
- Wired, or become worse, on antidepressants
Perinatal Psychosis
- Delusions and/or hallucinations
- Rambling speech
- Insomnia
- Confusion/Disorientation
- Rapid mood swings
- Waxing and waning (feel normal for stretches of time between the above symptoms)
- *Mom does not recognize that these actions/thoughts are unhealthy
Get Postpartum Support in St. Louis, MO
Reach out to Marble Wellness! Our Client Care Coordinator will be your first point of contact. She’ll get you set up with a good match for you on our team, and talk first appointment details. Meet with one of our Therapists for Moms! We have members of our team who are specifically trained in Maternal Mental Health, including Perinatal Mood & Anxiety Disorders. They will help you target specific ways to start feeling like yourself again! Start to live happy and calm again! Whether in-person, online, or park therapy, you and your therapist will use their skills and your strengths to help you start to live the life you’ve been longing for.
Other Services at Marble Wellness
Counseling services designed to help set you on a path of living a more fulfilled, calm, and happy life. We specialize in anxiety, depression, grief, chronic illness, therapy for men, couples, and maternal overwhelm. Our maternal mental health team can also help new moms with various postpartum concerns, moms in the thick of parenting, and moms with teens. We can also chat from wherever you are in the state with online therapy in Missouri and online therapy in Illinois. No matter where you are in your journey, we would love to support you.